Wilson’s disease is a genetic disorder that disrupts the body’s ability to eliminate excess copper. When left unmanaged, this accumulation can damage critical organs like the liver, brain, and eyes. Named after Dr. Samuel Alexander Kinnier Wilson, who first identified the condition, it often begins showing symptoms in childhood or early adulthood. With timely diagnosis and ongoing care, those affected can live a fulfilling life.
Causes of Wilson’s Disease
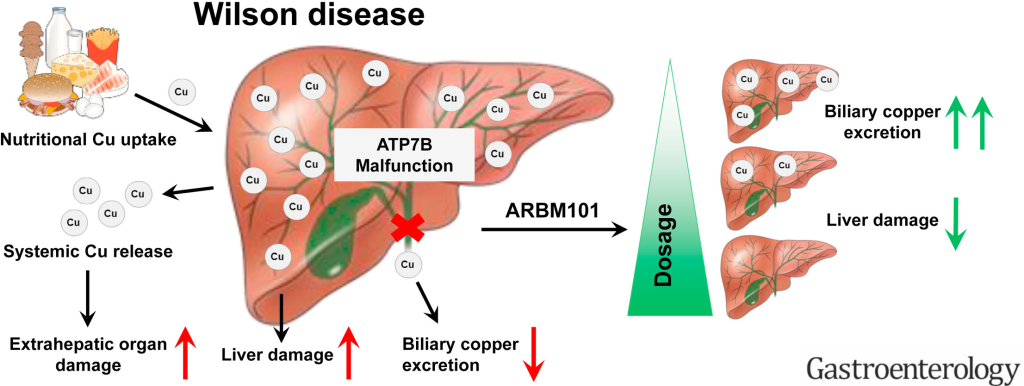
Wilson’s disease results from mutations in the ATP7B gene, which regulates copper transport. The inability to excrete copper leads to its accumulation in the liver and other organs.
- Genetic Inheritance: An autosomal recessive condition, meaning both parents must pass on the defective gene.
- Copper Imbalance: Excess copper builds up in the liver, brain, eyes, and kidneys, causing toxicity.
Indications of Wilson’s Disease
Early signs can be mistaken for other conditions, making awareness critical:
- Persistent fatigue or weakness.
- Yellowing of the skin and eyes (jaundice).
- Abdominal pain, swelling, or discomfort.
- Behavioral changes, including irritability and mood swings.
Symptoms of Wilson’s Disease
Symptoms vary based on the organs affected:
- Liver Symptoms: Jaundice, swelling, and liver failure.
- Neurological Symptoms: Tremors, difficulty with speech, and poor coordination.
- Psychiatric Symptoms: Depression, anxiety, or sudden personality changes.
- Ocular Symptoms: Kayser-Fleischer rings—copper-colored deposits around the cornea.
Prevention Strategies of Wilson’s Disease
Although Wilson’s disease is genetic and cannot be prevented, its progression can be controlled through:
- Genetic Screening: Early identification in families with a history of the disorder.
- Routine Testing: Monitoring copper levels for at-risk individuals.
- Dietary Management: Avoiding copper-rich foods like shellfish, liver, and nuts.
- Regular Medical Follow-Ups: Ensuring consistent treatment and monitoring for complications.
Myths and Facts About Wilson’s Disease
- Myth: Wilson’s disease only affects the liver.
Fact: It impacts multiple organs, including the brain and eyes. - Myth: Only adults develop Wilson’s disease.
Fact: Symptoms often appear in children or teenagers. - Myth: Copper-rich diets cause the disease.
Fact: It is a genetic disorder and not caused by dietary copper.
Treatments and Therapy
Medication-Based Treatments
- Chelating Agents: Penicillamine and trientine bind to copper, enabling its removal from the body.
- Zinc Therapy: Prevents copper absorption in the digestive tract.
Surgical Treatments
- Liver Transplantation: A last-resort option for severe liver damage.
Physical Therapy and Rehabilitation
- Helps improve motor skills and manage neurological impairments caused by copper buildup.
Lifestyle and Behavioral Interventions
- Maintaining a copper-restricted diet and staying hydrated supports overall health.
Alternative and Complementary Medicine
- Techniques like yoga and acupuncture may alleviate stress and improve quality of life.
Psychotherapy and Counseling
- Offers emotional support to help patients and families cope with the challenges of chronic illness.
Immunizations and Vaccines
- Protect against infections in individuals with compromised liver function.
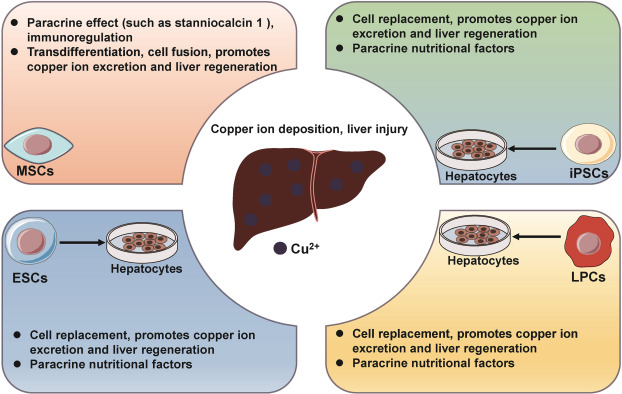
Stem Cell Therapy
- An area of ongoing research for repairing liver damage caused by copper toxicity.
Gene Therapy
- Experimental approaches aim to correct the ATP7B gene mutation, potentially offering a cure in the future.
Top 20 FAQ on Wilson’s Disease

1. What is Wilson’s disease?
It is a genetic disorder that leads to excess copper accumulation in the body, particularly in the liver, brain, and eyes, causing organ damage.
2. How is it diagnosed?
Wilson’s disease is diagnosed using:
- Blood tests to measure ceruloplasmin levels.
- Liver function tests.
- Genetic screening for ATP7B mutations.
- Eye examinations to detect Kayser-Fleischer rings.
3. What tests confirm the disease?
Tests like serum ceruloplasmin levels, 24-hour urine copper tests, and liver biopsy are key for confirming Wilson’s disease.
4. Can it be cured completely?
While there is no permanent cure, lifelong treatment can effectively control the disease and prevent complications.
5. Who is at risk?
Individuals with a family history of Wilson’s disease or whose parents both carry the ATP7B gene mutation are at higher risk.
6. Are there lifestyle changes needed?
Yes, lifestyle changes include:
- Adopting a low-copper diet.
- Regular medical check-ups to monitor copper levels and organ health.
- Strict adherence to prescribed medications.
7. What are Kayser-Fleischer rings?
These are copper deposits around the cornea, visible during an eye exam, and are a distinctive feature of Wilson’s disease.
8. How does it affect the brain?
Wilson’s disease can lead to:
- Neurological symptoms like tremors, slurred speech, and poor coordination.
- Psychiatric symptoms such as depression, anxiety, and mood swings.
9. Can it cause infertility?
Yes, untreated Wilson’s disease may cause hormonal imbalances and other complications that affect fertility.
10. How is it managed during pregnancy?
Treatment continues during pregnancy with adjusted medications to protect the mother and baby, often emphasizing zinc therapy.
11. What is the role of zinc in treatment?
Zinc therapy prevents copper absorption in the digestive system and helps maintain copper at safe levels.
12. Are there home remedies?
While a copper-restricted diet and staying hydrated can support medical treatment, they are not substitutes for prescribed therapies.
13. What foods should I avoid?
Avoid foods high in copper, including:
- Shellfish.
- Nuts.
- Chocolate.
- Liver.
14. How long does treatment last?
Treatment for Wilson’s disease is lifelong and requires ongoing monitoring and adherence.
15. What happens if untreated?
Without treatment, Wilson’s disease can lead to:
- Severe liver damage.
- Neurological complications.
- Death.
16. Can children develop it?
Yes, symptoms can appear in children, typically between the ages of 5 and 20.
17. Does it cause fatigue?
Yes, fatigue is a common symptom due to liver dysfunction and the toxic effects of copper buildup.
18. Is genetic testing mandatory?
Genetic testing is not mandatory but is highly recommended for at-risk families to identify carriers and affected individuals.
19. Are there new treatments available?
Research into gene therapy, stem cell therapy, and advanced medications is ongoing, offering hope for future breakthroughs.
20. Where can I get support?
Support is available through:
- Specialized clinics and hepatologists.
- Patient advocacy groups.
- Online forums and communities for those affected by Wilson’s disease.
Conclusion
Wilson’s disease is a challenging condition, but with early detection, proper medical care, and lifestyle changes, it can be effectively managed. Awareness and education are vital for ensuring a timely diagnosis and better outcomes for those living with the disease. If you or a loved one are at risk, consult a healthcare professional to take control of your health journey.
Your health is your power—start managing it today!
Related video: