Marfan Syndrome is a rare genetic disorder that affects the body’s connective tissue, which provides strength, elasticity, and support to various organs and structures. First described by French pediatrician Antoine Marfan in 1896, this condition can impact the heart, blood vessels, bones, joints, and eyes. While there is no cure, early diagnosis and effective management can significantly improve the quality of life for those living with Marfan Syndrome.
Causes of Marfan Syndrome
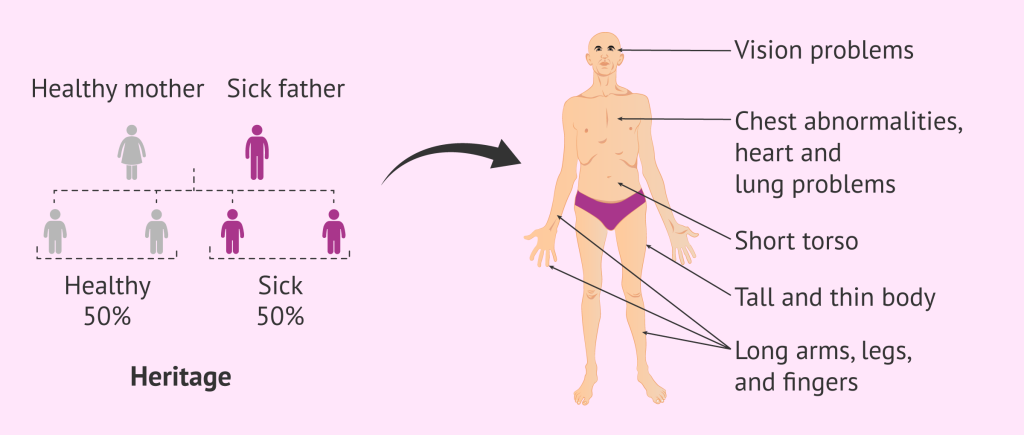
Marfan Syndrome is caused by a mutation in the FBN1 gene, which is responsible for producing fibrillin-1, a protein critical for connective tissue integrity. This mutation disrupts normal connective tissue development and function. The condition is typically inherited in an autosomal dominant pattern, meaning one copy of the mutated gene is enough to cause the disorder. However, in 25% of cases, the mutation arises spontaneously with no family history.
Indications of Marfan Syndrome
Early signs and characteristics that might indicate Marfan Syndrome include:
- A tall, slender build with disproportionately long limbs, fingers, and toes (arachnodactyly).
- Abnormal spine curvature, such as scoliosis or kyphosis.
- Chest deformities, such as a sunken (pectus excavatum) or protruding chest (pectus carinatum).
- Flexible joints.
- Vision problems due to dislocated lenses.
Symptoms of Marfan Syndrome
Symptoms vary widely depending on the severity and the systems affected. Common symptoms include:
- Cardiovascular System:
- Enlarged aorta (aortic aneurysm).
- Heart valve issues, such as mitral valve prolapse.
- Irregular heartbeat or arrhythmias.
- Skeletal System:
- Long limbs and fingers.
- Flat feet or overly flexible joints.
- Chest deformities or curved spine.
- Ocular System:
- Lens dislocation (ectopia lentis).
- Nearsightedness or early cataracts.
- Retinal detachment or glaucoma.
- Other:
- Stretch marks not associated with weight changes.
- Fatigue from musculoskeletal or cardiovascular strain.
Prevention Strategies for Marfan Syndrome
Since Marfan Syndrome is a genetic disorder, it cannot be prevented. However, steps can be taken to manage the condition and mitigate complications:
- Genetic Counseling: Families with a history of Marfan Syndrome should seek genetic counseling to understand the risks for future generations.
- Routine Monitoring: Regular cardiovascular, skeletal, and eye exams are essential for early detection of complications.
- Lifestyle Modifications: Avoid high-impact physical activities or sports that put excessive strain on the heart or joints.
Myths and Facts About Marfan Syndrome
- Myth: Marfan Syndrome only affects the heart. Fact: It impacts multiple systems, including the skeleton, eyes, and lungs.
- Myth: People with Marfan Syndrome are always extremely tall. Fact: While many individuals are tall, height alone is not diagnostic of Marfan Syndrome.
- Myth: There is no treatment for Marfan Syndrome. Fact: While there’s no cure, treatments and lifestyle adaptations can effectively manage symptoms.
- Myth: Marfan Syndrome is always inherited. Fact: While most cases are inherited, 25% result from spontaneous mutations.
Treatments and Therapy
Medication-Based Treatments
- Beta-blockers: Reduce blood pressure and strain on the heart to prevent aortic enlargement.
- Angiotensin Receptor Blockers (ARBs): Manage blood pressure and protect the aorta.
Surgical Treatments
- Aortic Surgery: For severe aortic dilation or rupture risk.
- Orthopedic Surgery: To correct severe scoliosis or chest deformities.
- Eye Surgery: For dislocated lenses or glaucoma.
Physical Therapy and Rehabilitation
- Tailored physical therapy programs can improve posture, muscle strength, and joint stability.
Lifestyle and Behavioral Interventions
- Engage in low-impact activities like swimming or walking.
- Avoid heavy lifting or competitive sports.
- Maintain a balanced diet to support bone and heart health.
Alternative and Complementary Medicine
Some patients explore yoga or acupuncture to manage stress and musculoskeletal pain. These should complement medical treatments, not replace them.
Psychotherapy and Counseling
- Emotional support can help individuals cope with chronic health challenges, stigma, or lifestyle adjustments.
Immunizations and Vaccines
- Staying up-to-date with vaccinations helps prevent infections that could worsen complications.
Stem Cell Therapy
- Currently experimental, research explores stem cell therapies to repair connective tissues.
Gene Therapy
- Future advancements may focus on correcting the FBN1 gene mutation to target the root cause of Marfan Syndrome.
Top 20 FAQ on Marfan Syndrome
1. What is Marfan Syndrome?
Marfan Syndrome is a genetic disorder that affects connective tissue, impacting various parts of the body such as the heart, skeleton, and eyes.
2. Is Marfan Syndrome hereditary?
Yes, it is hereditary in most cases, passed down in an autosomal dominant pattern. However, about 25% of cases arise from spontaneous mutations.
3. Can Marfan Syndrome be cured?
No, Marfan Syndrome cannot be cured, but symptoms and complications can be effectively managed with medical care and lifestyle adjustments.
4. What are the main symptoms?
Key symptoms include:
- Tall stature and long limbs.
- Aortic enlargement or dilation.
- Lens dislocation (ectopia lentis) and other vision issues.
- Scoliosis or chest deformities.
5. How is Marfan Syndrome diagnosed?
Diagnosis involves:
- A detailed physical exam.
- Imaging tests like echocardiograms or MRIs to check the heart and aorta.
- Genetic testing for mutations in the FBN1 gene.
6. What is the life expectancy?
With proper monitoring and treatment, individuals with Marfan Syndrome often live near-normal lifespans.
7. What is the most serious complication?
The most serious complication is aortic dissection or rupture, which can be life-threatening without prompt medical intervention.
8. Are children affected?
Yes, children can show symptoms early, such as tall stature, joint hypermobility, or vision problems. Early diagnosis is crucial for managing risks.
9. Is surgery common?
Surgery is typically reserved for severe complications, such as:
- Aortic repair to prevent rupture.
- Scoliosis correction.
- Eye surgeries for lens dislocation or cataracts.
10. Can it affect pregnancy?
Yes, pregnancy poses risks for individuals with Marfan Syndrome, particularly due to increased stress on the aorta. Close monitoring by a specialized healthcare team is essential.
11. Does it affect vision?
Yes, common vision issues include lens dislocation, nearsightedness, early cataracts, and an increased risk of glaucoma.
12. What sports are safe?
Low-impact sports like swimming, yoga, and walking are generally safe, while high-impact or contact sports should be avoided due to cardiovascular and joint risks.
13. Can Marfan Syndrome skip generations?
Rarely. Marfan Syndrome typically follows a dominant inheritance pattern, meaning it is passed directly from a parent to a child if the parent carries the mutated gene.
14. What treatments exist for heart problems?
Heart problems are managed with:
- Medications: Beta-blockers or angiotensin receptor blockers (ARBs) to reduce stress on the aorta.
- Surgery: Aortic repair or valve replacement in severe cases.
15. How common is Marfan Syndrome?
Marfan Syndrome affects approximately 1 in 5,000 people worldwide.
16. Can Marfan Syndrome cause mental health issues?
Yes, individuals may experience anxiety, depression, or social challenges related to managing a chronic illness or physical differences.
17. Is genetic testing available?
Yes, genetic testing can confirm mutations in the FBN1 gene, aiding in diagnosis and family planning.
18. Can lifestyle changes help?
Absolutely. Avoiding activities that strain the heart, maintaining a healthy weight, and regular checkups are key to managing the condition.
19. What’s the role of diet?
A balanced diet helps support overall health, particularly bone strength and cardiovascular wellness. Adequate calcium and vitamin D intake are recommended.
20. What research is underway?
Current research focuses on:
- Gene therapy to target the underlying genetic mutation.
- Stem cell research for connective tissue repair.
- Advanced surgical techniques to improve outcomes for aortic and skeletal complications.
Conclusion: Living Beyond Limits
Marfan Syndrome is a part of life, but it doesn’t have to define it. By understanding the condition and taking proactive steps, individuals can lead vibrant, fulfilling lives. From early diagnosis and medical care to emotional and social support, the path to thriving with Marfan Syndrome is built on awareness and action. Together with ongoing research and advancements, the future holds promise for those living with this condition.
Related video: